Women’s reproductive health issues like cervical cancer are often preventable and highly treatable if caught early. That’s why it’s crucial to get regular cervical cancer screenings and pelvic exams. However, there are lots of misconceptions about visiting the OB/GYN. We spoke to Dr. Julianne Kenton-Haney with Atrium Health Women's Care Creek Pointe OB/GYN to bust some common myths.
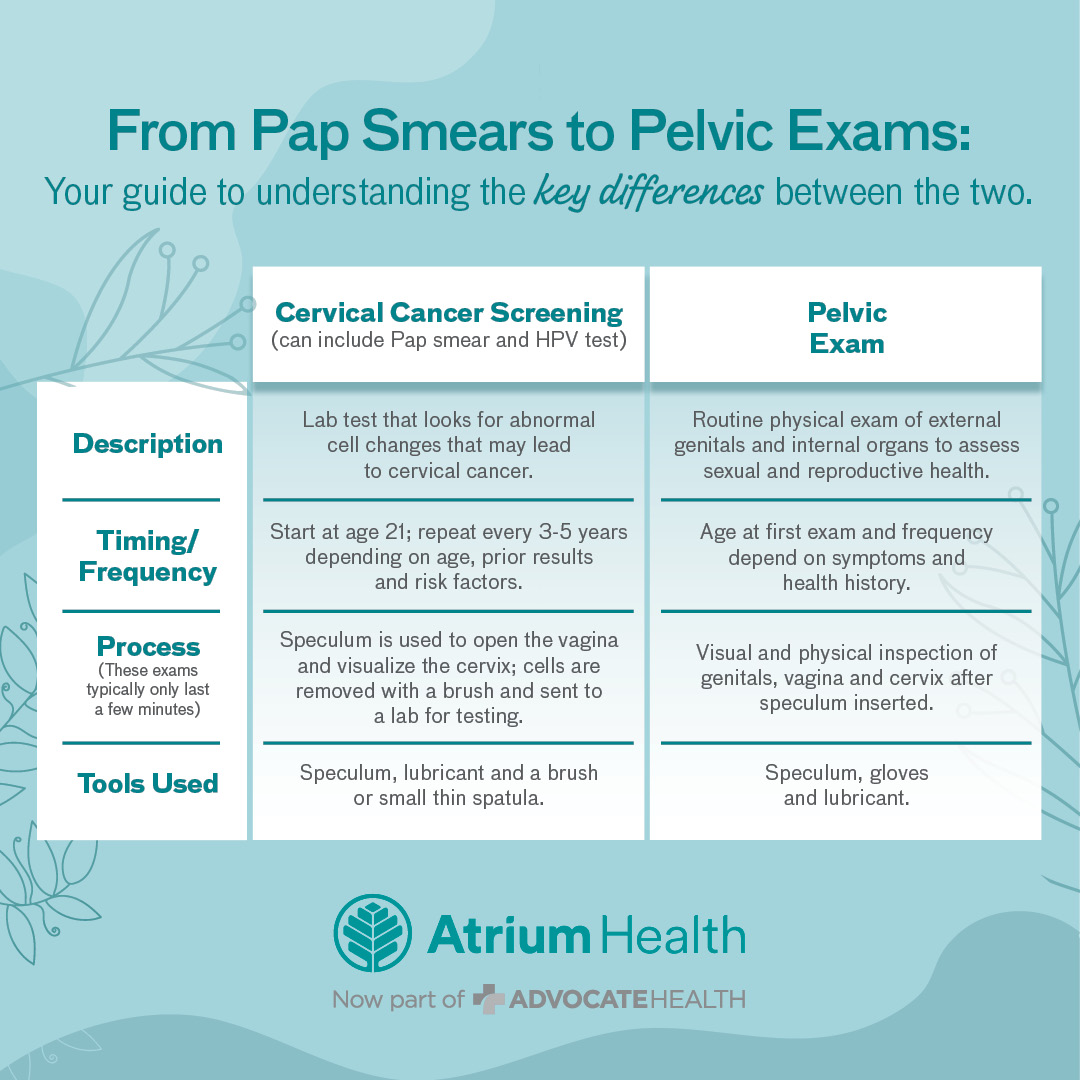
Myth: Cervical cancer screenings and pelvic exams are the same.
Fact: They’re different ways doctors assess women’s reproductive health. A cervical cancer screening, which may include a Pap smear and HPV test, is a lab test that looks for abnormal changes that lead to cervical cancer. During this screening, a provider will insert a speculum into the vagina and use a brush to remove cells that will be sent off for testing.
Experts recommend having a cervical cancer screening every three to five years (but this frequency may change based on your health history and risk factors).
A pelvic exam is typically an annual routine physical examination of the genitals and internal organs. During a pelvic exam, a provider will insert a speculum and visually inspect the vagina and cervix.
 |
Myth: You don’t need to go to the gynecologist every year.
Fact: Dr. Kenton-Haney says this the #1 misconception among women.
“You may not need a Pap smear every year, but we will perform a breast and pelvic exam,” Dr. Kenton-Haney says. “Even if you don’t notice any symptoms or have any women’s health issues, it’s a great opportunity to discuss your menstrual cycle, reproductive health or peri-post menopausal issues.”
Since early detection could be life-saving, seeing your OB/GYN regularly is the best way to take control of your reproductive health.
Myth: You don’t need to start seeing an OB/GYN until age 21.
Fact: The earlier you start developing a relationship with an OB/GYN, the better. Although Pap smears and pelvic exams aren’t typically done on patients younger than 21 unless requested or needed, seeing an OB/GYN earlier is a good idea. “You can start developing a relationship … to become more educated regarding menstrual cycles, STDs, safe sex and pregnancy prevention,” Dr. Kenton-Haney says.
Myth: Going to the OB/GYN is always uncomfortable.
Fact: Providers do everything in their power to prevent anxiety and discomfort.
“We won’t do anything that makes you uncomfortable. We can talk you through what will happen during the exam,” Dr. Kenton-Haney says. “Honestly, I find the fear of the unknown or anticipation of the exam is much worse than reality,”
The bottom line: don’t let fear or nervousness cause you to avoid seeking care.
Early detection is crucial. You should see your OB/GYN as soon as possible if you have acute symptoms like abnormal vaginal bleeding, postmenopausal bleeding, bumps or blisters, unusual vaginal discharge, vaginal odor or breast concerns.
If you need help finding an OB/GYN, check out Atrium Health's online provider directory and schedule an appointment.